Abstract
BACKGROUND: Polycythemia Vera (PV) is a myeloproliferative neoplasm characterized by uncontrolled proliferation of erythrocytes with frequent co-stimulation of myeloid and megakaryocyte progenitor cells. Prior to the utilization of molecular testing, subnormal or low erythropoietin (EPO) levels were an important component in the diagnosis of PV. In 2005, the somatic JAK2 V617Fmutation was discovered to be present in greater than 95% of patients with PV. In turn, the 2008 WHO diagnostic criteria revision added the JAK2 mutation to the major criteria. The current WHO criteria for the diagnosis of PV designates the major criteria to be a hemoglobin greater than 16.5 g/dL in men and 16 g/dL in women (or a hematocrit greater than 49% in men and 48% in women), a bone marrow biopsy demonstrating hypercellularity and trilineage panmyelosis, and the presence of a JAK2 V617F or exon 12 mutation. A subnormal EPO level is a minor criterion. Based on these, PV can be diagnosed by the presence of all three major criteria, or the first two major criteria with a subnormal EPO level.
Subnormal EPO levels have been reported to be found in only around 30% of patients otherwise meeting the diagnostic criteria for PV. The sensitivity and specificity of a subnormal EPO level in the diagnosis of PV has been shown to be 64% and 96%, respectively. The diagnostic value of the EPO level is confounded by the co-occurrence of comorbidities such as obstructive sleep apnea, chronic obstructive pulmonary disease, tobacco use, and obesity. As a result, controversies exist as to the role of EPO in the diagnosis of PV. In this study, we aimed to describe the EPO level in patients with primary erythrocytosis (or PV) and secondary erythrocytosis in a Los Angeles safety-net hospital where these comorbidities are prevalent. We also examined the prevalence of these comorbidities in both patient populations.
METHODS: We performed a retrospective chart review of all patients aged greater than 18 years who presented to Harbor-UCLA Medical Center between 2015 and 2021 with the diagnosis of erythrocytosis using the International Classification of Disease-specific codes. We excluded patients who were erroneously given the diagnosis code for erythrocytosis when no erythrocytosis was documented or patients who had one documented hemoglobin level above the normal reference range with spontaneous resolution and no further work up. Patient demographics, baseline characteristics, laboratory values, bone marrow biopsy results, molecular testing, and comorbidities were recorded.
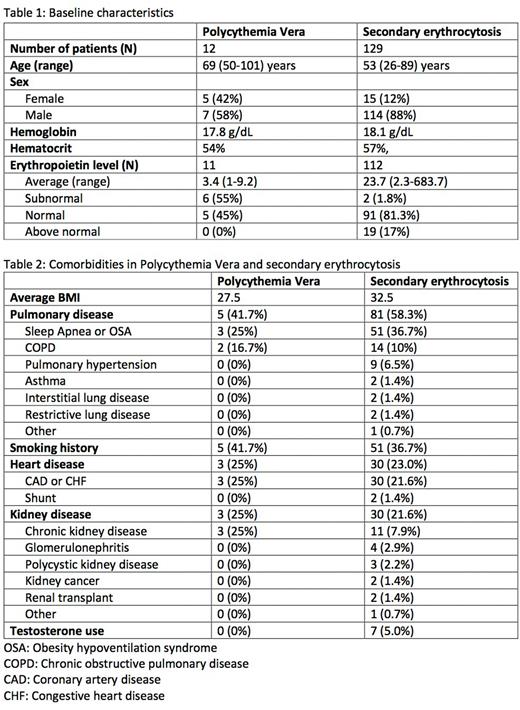
RESULTS: There was a total of 141 patients who met the inclusion criteria (Table 1). Of these, 12 (8.5%) had the diagnosis of primary erythrocytosos or PV. Of those diagnosed with PV, all 12 (100%) had the JAK2 V617Fmutation. The average hemoglobin and hematocrit of patients with PV and secondary erythrocytosis was 17.8 g/dL and 54% and 18.1 g/dL and 57%, respectively. The average EPO for those with primary and secondary erythrocytosis was 3.4 mIU/mL and 23.7 mIU/mL, respectively (normal 2.6-18.5 mIU/mL). Of those with primary polycythemia, 6/11 (55%) had a subnormal EPO level at diagnosis. The average age of those with PV and secondary erythrocytosis was 69 years and 53 years, respectively. The average BMI for those with PV and erythrocytosis was 27.5 and 32.5, respectively. In those with secondary erythrocytosis versus PV, the most common comorbidities were pulmonary disease (58.3% versus 41.7%), smoking (36.7% versus 41.7%), heart disease (23.0% versus 25%), kidney disease (21.6% versus 25%), and testosterone use (5.0% versus 0%) (Table 2).
CONCLUSIONS: In this study, we found that most patients with PV had a low EPO level at diagnosis with over half having a subnormal EPO level. In contrast, very few patients with secondary erythrocytosis had a subnormal EPO level. The prevalence of comorbidities was common in both primary and secondary erythrocytosis.
Disclosures
Tomassetti:Novartis: Research Funding; Beigene: Research Funding; Rigel: Research Funding; SeaGene: Research Funding; Merck: Research Funding; Principia: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal